Key Takeaways
- MSOs and DSOs offer different approaches to practice management, impacting ownership, control, and compliance requirements.
- Legal and regulatory considerations are essential when structuring MSO or DSO agreements to avoid violations and ensure smooth operations.
- The right model can improve growth, operational efficiencies, and scalability, but practicing due diligence is critical.
Table of Contents
- Defining MSOs and DSOs
- Key Differences Between MSOs and DSOs
- Benefits of MSO and DSO Models
- Legal Considerations
- Recent Trends and Developments
- Conclusion
Defining MSOs and DSOs
As the healthcare industry evolves, medical practices must find ways to improve administrative efficiency while maintaining clinical excellence. Two organizational models that have emerged to address these requirements are Management Services Organizations (MSOs) and Dental Support Organizations (DSOs). The distinction between these two models can influence key operational outcomes for healthcare providers considering a change or expansion in their business structure. For tailored legal insight on these and other complex regulatory structures, healthcare practices can consult legal professionals at dklawg.com to ensure all management and ownership decisions are sound and compliant.
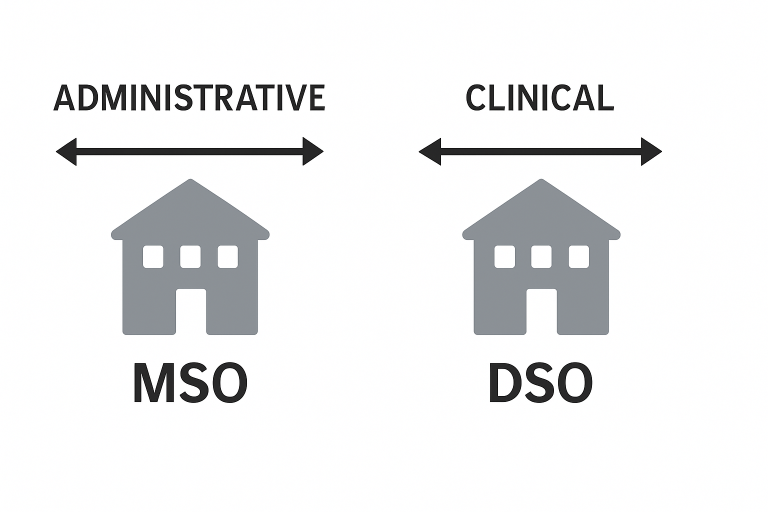
An MSO typically provides non-clinical support services, including billing, IT, marketing, compliance, and human resources. The clinical aspects and ownership of the professional entity remain with licensed practitioners, such as physicians or dentists. This separation allows the practice to comply with the corporate practice of medicine doctrine, which prohibits non-physicians from owning or controlling the clinical portion of a medical practice.
On the other hand, the DSO model is commonly used in the dental industry but can be applied to other healthcare practices in states that allow corporate ownership. DSOs are structured to own, operate, or directly control both the clinical and non-clinical activities of the practice. They often manage business functions such as payor contracting, real estate acquisition, procurement, and multi-site expansion strategy, leveraging their larger scale.
This nuanced difference means that DSOs frequently play a more direct role in practice leadership, sometimes influencing clinical workflows or growth strategies. Both organizational types are designed to unburden healthcare providers from administrative distractions, but the level of control and legal compliance requirements can differ significantly.
For a broader overview of MSO and DSO options and related considerations, additional information is available from resources such as the American Medical Association.
Key Differences Between MSOs and DSOs
- Ownership and Control: Under the MSO model, clinical decision-making and legal ownership remain with licensed practitioners. The MSO supplies business support without infringing on clinical independence. Conversely, a DSO may take an ownership stake in the practice if state law allows, potentially centralizing both business and some clinical leadership functions.
- Compliance with Law: An MSO helps practices comply with corporate practice restrictions that prevent non-physicians from controlling medical entities. DSOs are often viable only in jurisdictions where corporate or non-physician ownership is permissible under state regulations.
- Scope of Services: While MSOs primarily handle back-office tasks, DSOs take on a broader operational portfolio, often encompassing direct clinical management, marketing, strategy, and vendor negotiations.
Benefits of MSO and DSO Models
Whether choosing an MSO or a DSO model, medical practices can realize substantial gains in efficiency, profitability, and scalability. Administrative consolidation enables practices to devote more time to patient care and less to time-consuming business matters. Access to professional support in HR, compliance, accounting, and information technology reduces administrative headaches and streamlines workflow.
- Administrative Relief: Both MSOs and DSOs provide comprehensive support, enabling physicians to spend less time managing operations and more time focusing on patients.
- Economies of Scale: Larger organizations can negotiate better service rates, purchase supplies at volume discounts, and leverage shared resources to lower average operational costs.
- Access to Growth Capital: DSOs, and to some degree MSOs, facilitate access to funding for upgrades, new equipment, expansion projects, and technology investments, making them appealing to groups with ambitions for regional or multi-state growth.
In addition, practices partnering with DSOs or MSOs often see improvements in compliance, risk management, and staff recruitment, thanks to established procedures and professional oversight.
Legal Considerations
Engaging in a relationship with an MSO or DSO carries significant legal implications. To comply with state and federal law, MSO contracts must clearly separate clinical and business functions. Violations of the corporate practice of medicine doctrine can result in civil and regulatory penalties for both the provider and the business management entity. Similarly, any fee-splitting arrangement must avoid inadvertent exposure under statutes like the Stark Law or the federal Anti-Kickback Statute. Healthcare business leaders are strongly encouraged to seek guidance from legal counsel before entering into any MSO or DSO arrangement.
According to Modern Healthcare, oversight and enforcement in this arena are increasing, particularly with more private equity-backed consolidations and multistate operations. Careful structuring and ongoing compliance monitoring are vital for a successful venture.
Recent Trends and Developments
In recent years, there has been a marked increase in private equity investors expressing interest in scalable healthcare and dental models, leading to a surge in both MSO and DSO formations. Investors are particularly focused on models that enable robust growth, predictable income streams, and network expansion. Practices considering these organizational changes should thoroughly vet potential partners, evaluating their track record, fee structures, compliance oversight, and alignment with the practice’s culture and long-term objectives.
This trend is also leading to a shift in the competitive landscape of the healthcare industry, with consolidation driving innovation but also spurring greater regulatory scrutiny. Healthcare providers should remain vigilant about evolving industry standards and prepare for increased competition from larger, well-funded networks.
Conclusion
Choosing between an MSO and a DSO is a significant decision that depends on state law, practice goals, and desired balance of control and support. Medical providers in Texas and elsewhere should undertake comprehensive due diligence before moving forward. Consulting experienced healthcare attorneys and financial advisors helps ensure the chosen path supports long-term clinical, compliance, and economic success.